Abstract
Background:
Timely anticoagulant (AC) initiation is critical in patients with newly diagnosed venous thromboembolism (VTE) to avert recurrence and associated mortality. However, data on the impact of anticoagulant timing on clinical outcomes in sickle cell disease (SCD) patients with newly diagnosed VTE are scarce.
Objective:
To assess the impact of delayed AC initiation on clinical outcomes in SCD patients with newly diagnosed VTE.
Methods:
We conducted a retrospective matched-cohort study using the 2009-2015 Truven Health MarketScan® databases to identify subjects with newly diagnosed VTE (VTE diagnosis date used as the index date) and SCD based on International Classification of Diseases (ICD) codes for inpatient and outpatient encounters. VTE patients with SCD were 1:5 individually matched to non-SCD patients on sex, age, index date, and VTE type. Timing of AC initiation was defined as: (a) timely initiation (treatment started within 24 hours post index; reference group), (b) delayed initiation (treatment started within 2-7 days post-index) and (c) no treatment (treatment not started within 7 days post-index). Clinical outcomes were defined as: (i) effectiveness endpoint (time to recurrent VTE), (ii) safety endpoint (time to clinically relevant bleeding) and (iii) composite endpoint (first recurrent VTE or clinically relevant bleeding) within 365 days post index.
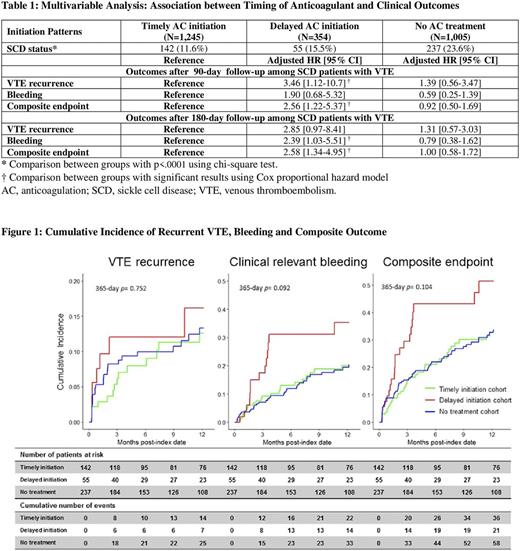
Kaplan-Meier survivor functions were estimated for all three endpoints by anticoagulant initiation patterns and censored for end of continuous enrollment, end of observation period and occurrence of the opposite outcome. Multivariable Cox proportional hazards models were used to compare hazard ratios (HRs) between groups with adjustment for potential confounders.
Results:
We identified 434 SCD patients and 2170 non-SCD controls with newly diagnosed VTE. The median age was 45 years (range 15-98) and 63.4% were female. Compared to non-SCD patients, timely initiation of AC therapy was significantly lower in those patients with SCD (50.8% vs 32.7%, p<0.0001). Further, in the SCD cohort, 142 (32.7%) patients had timely AC initiation, 55 (12.7%) had delayed AC initiation and 237 (54.6%) had no AC initiated within 7 days post-index. VTE recurrence and/or bleeding occurred in 36/142 (25.4%) patients with timely AC initiation versus 21/55 (38.2%) with delayed initiation and 59/237 (23.2%) with no AC initiation (p=0.1). (Figure 1) In multivariable analyses, delayed AC was associated with higher risk of VTE recurrence compared to those with timely AC initiation (HR [95% CI] = 3.46 [1.12-10.7]) within 90 days post index. Within 180 days post index, results remained suggestive of increased risk of VTE recurrence (HR [95% CI] = 2.85 [0.97-8.41]) and significantly higher risk of clinically relevant bleeding (HR [95% CI] = 2.39 [1.03-5.51]). Delayed anticoagulation was associated with significantly greater risk of the composite outcome compared to those with timely anticoagulant initiation (HR [95% CI] = 2.56 [1.22-5.37] and 2.58 [1.34-4.95]) within 90 and 180 days post index, respectively. We did not find an association in relation to outcomes between those with timely AC initiation and those with no AC initiation within 7 days post index. (Table 1)
Conclusions:
It is of concern that SCD patients with a newly diagnosed VTE were less likely to receive timely AC initiation. Delayed AC initiation in SCD patients was associated with greater risk of VTE recurrence and clinically significant bleeding at 90 and 180-days post index, respectively. Paradoxically, we found no statistically significant difference in clinical events between those with timely AC initiation and no AC initiation within 7 days post index. This discrepancy may be attributed to provider preferences in terms of risk-benefit guided treatment initiation and differential event reporting in those without a record of AC initiation in our database. Further investigation is warranted to evaluate provider treatment initiation preferences in relation to patient risk and AC treatment patterns vs risk-benefit balance in SCD patients with VTE.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal